
Therapeutic Use of Oxygen for Chronic Wounds
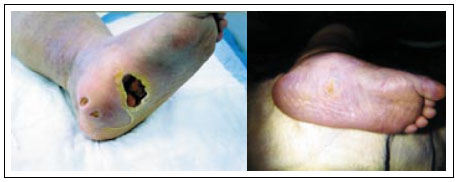 Chronic wounds, like venous leg and diabetic foot ulcers (see right), are wounds that do not heal in a timely fashion, generally two-to-four weeks. Chronic wounds can cause pain and discomfort and also limit mobility. They are often a consequence of a more serious health problem, such as diabetes, heart disease, or blood circulation disorders. Left untreated, chronic wounds can lead to problems like infection, amputation, or even death. At the same time, the cost of treatment can be staggering, estimated to be $5-10 billion annually effecting more than one million Americans.
Chronic wounds, like venous leg and diabetic foot ulcers (see right), are wounds that do not heal in a timely fashion, generally two-to-four weeks. Chronic wounds can cause pain and discomfort and also limit mobility. They are often a consequence of a more serious health problem, such as diabetes, heart disease, or blood circulation disorders. Left untreated, chronic wounds can lead to problems like infection, amputation, or even death. At the same time, the cost of treatment can be staggering, estimated to be $5-10 billion annually effecting more than one million Americans.
Wounding disrupts the vascular network at the wound site, which causes the wound micro-environment to be hypoxic. The lack of oxygen in the wound can cause the wound to become chronic. Low levels of oxygen can increase the risk of infection, limit broblast growth and growth-factor production, and impair angiogenesis, which in the formation of blood vessels from existing vasculature. To promote the healing response of the tissue, doctors increase the oxygen concentration in the wound by administration of hyperbaric oxygen and by application of topical oxygen gas. Yet, ways to optimize the use of hyperbaric or topical oxygen, such as levels of oxygen concentration and frequency and duration of administration, are poorly understood as clinical success of these treatments varies.
In a collaboration between MBI Postdoctoral Fellow Richard Schugart, MBI Director Avner Friedman, and Director of the Comprehensive Wound Center at The Ohio State University Medical Center Chandan Sen, they have sought to find optimal oxygen-dosing strategies to best promote dermal wound angiogenesis. Through this collaboration, a mathematical model was developed, which consists of seven partial differential equations. The model takes into account many of the established biological components that contribute to the complex nature of wound healing, including the recruitment of inflammatory cells, chemo-attractants, endothelial cells, oxygen tension, and the build up of extracellular matrix in the wound region. Simulations from the model (see Figure 2) agree with a variety of experimentally-observed results, which include: (i) extreme hypoxia cannot sustain the growth of functional vessels; (ii) hyperoxia promotes wound angiogenesis and healing; (iii) extreme hyperoxia derails tissue repair and causes oxygen toxicity; (iv) intermittent oxygen treatment may stimulate an angiogenic response. Ongoing and future work includes further exploration for optimal treatments with oxygen and expansion of the list of factors as the biological complexities continue to be experimentally unveiled.
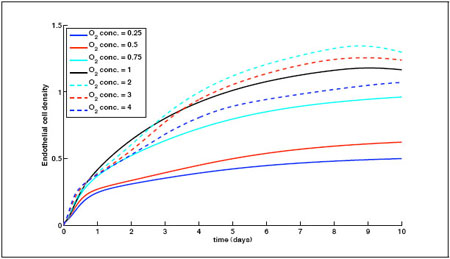
Figure 2: Endothelial cell density for different normalized oxygen concentrations through use of a hyperbaric oxygen chamber. Oxygen concentrations less than one are hypoxic, while oxygen concentrations greater than one are hyperoxic. The figure shows that the average endothelial cell density increases with oxygen level from hypoxic con- centrations above 0.5 to hyperoxic concentrations below 2. When the hypoxic level is below 0.5, the wound is sufficiently hypoxic and vessel growth does not occur. When the hyperoxic level is above 2, the wound becomes extremely hyperoxic and derails tissue repair. (From Schugart, R.C., Friedman, A., Zhao, R., Sen, C.K., Wound angiogenesis as a function of tissue oxygen tension: a mathematical model, PNAS USA 105: 2628 – 33, 2008.)