
Modeling the Prevention and Reversal of Type 2 Diabetes
Obesity raises the risk of diabetes by causing resistance to insulin, a hormone secreted by the beta cells of the pancreas that is central to utilization of glucose (G) as a fuel by cells. If resistance is not overcome by increased secretion from the beta cells, high blood sugar (diabetes) results. This damages multiple organs and leads to premature morbidity and death. The key question is, why are most obese individuals insulin resistant but not diabetic? The model of Sherman and Ha builds on a pioneering model developed in 2000 to address this question by physiologists Bryan Topp and Diane Finegood and their mathematics colleagues Robert Miura and Gerda de Vries. Those authors, motivated by earlier experimental evidence, proposed that when insulin secretion is inadequate to control G levels, the high G causes beta cells to proliferate, increasing the insulin levels and protecting most obese people from diabetes. However, if G rises beyond a threshold, it causes beta cell death, not proliferation. The system thus tips from negative feedback to positive feedback.
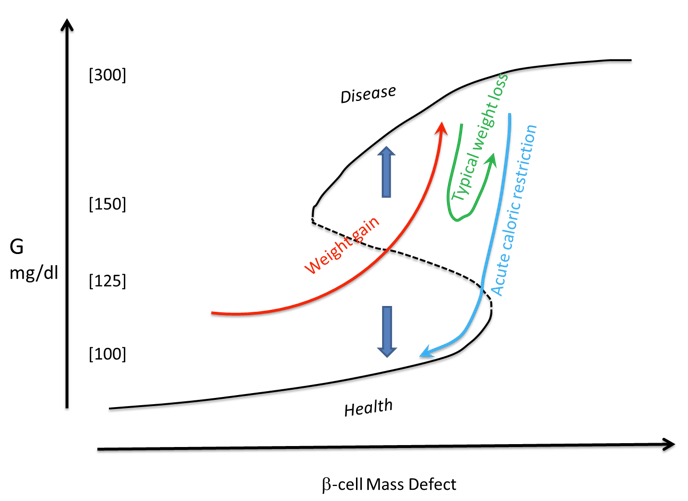 Recent data from Yuval Dor and colleagues suggest, however, that G per se is not the signal for proliferation, but rather beta-cell workload (secretion per cell). Sherman and Ha incorporated this into an extended model and showed that control of workload naturally leads to control of G by increase of beta-cell mass. Indeed, workload is an order of magnitude more sensitive as an indicator of insulin resistance than G because secretion rises much more after meals. The bifurcation diagram of the system (shown schematically in the figure) also clarifies the disease process. If people gain weight over time, they become insulin resistant, which not only increases the demand for insulin but hinders beta-cell proliferation. The metabolic state follows the red arrow up and to the right. Until the threshold (dotted line) is crossed, beta cell proliferation is adequate to combat high glucose (downward blue arrow). In this pre-diabetic phase, it is sufficient to stop getting worse by improving diet and exercise. Once the threshold is crossed, however, there is a net loss of beta cells and diabetes ensues. Reversal of the disease now requires a strong and rapid decline in G or improvement of insulin resistance to overcome the tendency for G to keep increasing (upward blue arrow). Typically achievable weight loss by diet and exercise is too slow and almost always fails (green arrow). Only acute caloric restriction by, for example, invasive bariatric surgery can bring the patient back below threshold to the healthy range (cyan arrow). The model informs the search for non-invasive cures by showing that, whatever the molecular mechanism, successful therapy requires a sharp reset of the system. The model also accounts for why prevention of T2D is much easier than cure and may be useful for reinforcing public service messaging to promote prevention.
Recent data from Yuval Dor and colleagues suggest, however, that G per se is not the signal for proliferation, but rather beta-cell workload (secretion per cell). Sherman and Ha incorporated this into an extended model and showed that control of workload naturally leads to control of G by increase of beta-cell mass. Indeed, workload is an order of magnitude more sensitive as an indicator of insulin resistance than G because secretion rises much more after meals. The bifurcation diagram of the system (shown schematically in the figure) also clarifies the disease process. If people gain weight over time, they become insulin resistant, which not only increases the demand for insulin but hinders beta-cell proliferation. The metabolic state follows the red arrow up and to the right. Until the threshold (dotted line) is crossed, beta cell proliferation is adequate to combat high glucose (downward blue arrow). In this pre-diabetic phase, it is sufficient to stop getting worse by improving diet and exercise. Once the threshold is crossed, however, there is a net loss of beta cells and diabetes ensues. Reversal of the disease now requires a strong and rapid decline in G or improvement of insulin resistance to overcome the tendency for G to keep increasing (upward blue arrow). Typically achievable weight loss by diet and exercise is too slow and almost always fails (green arrow). Only acute caloric restriction by, for example, invasive bariatric surgery can bring the patient back below threshold to the healthy range (cyan arrow). The model informs the search for non-invasive cures by showing that, whatever the molecular mechanism, successful therapy requires a sharp reset of the system. The model also accounts for why prevention of T2D is much easier than cure and may be useful for reinforcing public service messaging to promote prevention.